Varicocele
What is a Varicocele?
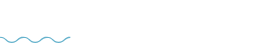
A varicocele is a collection of swollen veins in the scrotum. It is a common condition, occurring in about 15% of young men, and usually causes only minor symptoms. In some men, however, a varicocele is associated with more severe pain which can be troublesome and interfere with normal activities.
Varicoceles can also be associated with reduced fertility and are therefore commoner in those men suffering from fertility problems. Varicoceles occur because of a problem with the valves in the veins which carry blood from the scrotum and testicles. The condition, therefore, shares some similarities with varicose veins in the legs, and pelvic congestion syndrome in females.
Image credit: Mayo Clinic
The Symptoms of Varicoceles
A varicocele often produces no signs or symptoms so it can be difficult to know if you have one. Sometimes, you may feel pain or discomfort. So, how do you know if you have a varicocele? Other symptoms include:
- A Dull Ache in the Testicles
- A Feeling of Heaviness in the Testicles
- Visibly Swollen Veins
- Visibly Smaller Testicle
- Infertility
We are often asked, "what does a varicocele look like?" Over time, a varicocele grows and become more noticeable. Varicoceles usually have a 'twisted' appearance (see the above image) and have sometimes been described as looking like a ‘bag of worms’, and the condition might cause a swollen testicle - usually the left side.
Knowing when it’s time to see a doctor can be tricky, since you may not have any symptoms. As such, varicoceles often require no treatment, unless you are in pain or experiencing issues with fertility.
However, a swollen testicle is never a good sign, and you should speak with your doctor immediately if you have pain or notice a change in size to your scrotum.
.png?width=707&height=1000&name=Untitled%20design%20(24).png)
What Can Cause a Varicocele?
Varicoceles occur because of a problem with the valves in the veins which carry blood from the scrotum and testicles.
A spermatic cord, within the pampiniform plexus, holds up each testicle, and this cord contains the veins, arteries, and nerves that support the testicles. In healthy veins, one-way valves move the blood from the testicles back to the heart.
When "leaky", these valves do not return the blood back to the heart as they should and this causes a buildup of pressure, and therefore swollen veins, and a varicocele develops slowly over time. They are more common on the left side of the scrotum as the left testicular vein is more prone to valve problems.
Despite this, there are no established risk factors for developing a varicocele, and the exact cause of varicoceles is still unclear. We know it is due to problems with the valves, but we aren't sure why they develop.
Why Do Varicoceles Appear on the Left Side?
Varicoceles are usually more common on the left side of the scrotum, with approximately 90% of cases being left-sided. This is because your body is organised in a way that means more blood flows on the lefthand side. Greater blood flow means more chance of a varicocele developing, which is why they are frequently diagnosed on the left side.
In about 10-20% of cases we'll see bilateratel varicoceles, meaning it affects both the left and right side. Isolated right-sided varicoceles are rare, and usually require additional imaging to rule out retroperitoneal pathology, which refers to underlying issues or abnormalities located behind the abdominal cavity.
While most right-sided varicoceles are harmless, their presence can sometimes suggest that something else may be pressing on or affecting the veins in this area, such as a mass or growth, and that’s why doctors recommend further imaging like an ultrasound or CT scan to rule out any serious conditions. This ensures the cause of the varicocele is properly understood and managed, prioritising your overall health and wellbeing.
How Common are Varicoceles?
Varicoceles are actually quite common, affecting around 15% of all men. Many men are unaware they even have a varicocele because most cases don’t cause any pain or noticeable symptoms, and they are rarely dangerous. Often, people might only discover they have one during a routine check or when investigating other health concerns.
However, the significance of varicoceles increases when it comes to fertility. Among men dealing with infertility, up to 40% will be found to have a varicocele, making this condition the most common and treatable cause of male infertility. This is crucial information for couples trying to conceive, as addressing a varicocele can sometimes restore fertility.
Varicoceles tend to appear most often during adolescence, usually between the ages of 15 and 25. This is a vital period for physical development, and changes in blood flow during these years may increase the risk. If you’re experiencing any discomfort or notice changes, it’s always best to check in with your GP for advice and an accurate diagnosis. Early awareness and management can help protect your reproductive health and wellbeing.
Do Varicoceles Go Away on Their Own?
Unfortunately, varicoceles do not resolve on their own. If you want to get rid of a varicocele, some form of medical procedure is required, such as embolisation or surgery. That said, many men live comfortably with a varicocele and don’t need any treatment, especially if there’s no pain or effect on fertility. Your doctor will help you decide if any action is needed based on your personal symptoms and health goals. For some, simply monitoring the condition is all that’s required, while others may opt for intervention to improve comfort or fertility outcomes.
What are the Risk Factors for Developing Varicoceles?
Several factors may put someone at greater risk of developing a varicocele:
Anatomical predisposition
The main reason they occur more often on the left side is due to the body’s natural anatomy - specifically, the left spermatic vein connects to the left renal vein at a right angle, making backflow of blood more likely in this area. This means that blood can pool in the veins more easily, increasing the chances of varicocele formation.
Body type
Certain body types also play a role. Tall and thin males are at increased risk, because they tend to have longer veins in the scrotum, which can raise venous pressure and make it easier for the valves to falter.
Lifestyle factors
Activities that involve heavy lifting or straining, such as regular gym workouts, athletic training, or physically demanding jobs, can add extra pressure on the veins in the scrotum. Similarly, spending long periods standing up may contribute to higher venous pressure and elevate your risk. Even everyday factors like chronic constipation, frequent weightlifting, or regularly wearing very tight clothing can increase the pressure inside your abdomen, possibly making varicoceles more likely.
Family history
While these elements may heighten risk, varicoceles can also run in families. If you have a family history of weak veins or connective tissue disorders, or if your veins have naturally weaker valves, you may be more predisposed to developing varicoceles. Understanding these risk factors doesn’t mean you will definitely get a varicocele, but it can help you make informed decisions about your health and seek advice early if you experience symptoms.
Do Varicoceles Affect Testosterone?
A 2011 study did find that varicoceles can reduce testosterone production. The study looked at 325 men with a varicocele and compared their testosterone levels with 510 men who did not have a varicocele and found that, regardless of age, varicoceles have a statistically significant impact on testosterone levels. This study confirmed the findings of a 1992 World Health Organisation multicentre study that found varicocele presence correlates with lower testosterone in men over 30.
Recommended Reading: Examining the Relationship Between Varicoceles and Testosterone
Varicoceles and Infertility
There is ongoing debate, but there is strong evidence that varicoceles can contribute to infertility, though this only affects a small proportion of men with the condition. Around 10% to 20% of men diagnosed with a varicocele may experience difficulty fathering a child.
The underlying reason for infertility is not fully understood, but research has shown that many men who are infertile also have a varicocele. This overlap has led experts to suspect that varicoceles can negatively impact sperm quality, such as by reducing sperm production, impairing sperm movement (motility) and shape (morphology), and increasing sperm DNA fragmentation. However, it’s also common for varicoceles to simply coexist with other factors that cause low semen quality, without being the direct cause themselves.
Encouragingly, treating a varicocele can improve fertility outcomes for some men. Studies show that after treatment, semen parameters often improve within three to six months, and spontaneous pregnancy rates may rise by about 30–40% for select couples. Beyond fertility, varicoceles can also impact hormone levels. Over time, untreated varicoceles may reduce the function of Leydig cells, which are responsible for producing testosterone. This can lead to symptoms of low testosterone, including fatigue, low libido, and mood changes. The good news is that addressing the varicocele—either through embolisation or surgery—has been shown in some studies to improve testosterone production, especially in older men experiencing low testosterone. Many men also report an improvement in their symptoms following treatment.
How is a Varicocele Diagnosed?
You can check for a varicocele yourself by performing a physical examination, paying attention to swollen veins which have been described as feeling like a 'bag of worms'. If you feel something you think is abnormal, you can then make an appointment with your GP.
Diagnostic workflow
Diagnosing a varicocele starts with a thorough history and physical examination. Your doctor will ask about any pain, feelings of heaviness, or fertility concerns. During the exam, they’ll palpate your scrotum while you’re standing, both with and without a Valsalva manoeuvre (which involves you taking a deep breath and bearing down). Varicoceles are often missed if the exam is performed while you’re lying down, so standing is essential for accuracy.
If there is suspicion of a varicocele, the next step is a scrotal ultrasound. This imaging test is the gold standard for diagnosing varicoceles. It can confirm the presence of dilated veins, usually those wider than 2.5–3 mm, as well as detect retrograde blood flow during a Valsalva manoeuvre and spot any differences in testicular volume.
For men who are concerned about fertility, a semen analysis is also recommended. This test evaluates sperm count, motility (movement), and morphology (shape). Sometimes, a more advanced test called a DNA fragmentation index can be done to get a deeper understanding of sperm health.
If there are signs of hypogonadism (low testosterone), or if infertility is an issue, a hormonal evaluation may be suggested. This typically involves measuring your total testosterone as well as follicle-stimulating hormone (FSH) and luteinising hormone (LH) to get a clearer picture of your reproductive health.
Finally, if an isolated right-sided varicocele is detected, your doctor might recommend more advanced imaging—such as an abdominal CT or MRI—to rule out any compression or mass that could be contributing to the condition.
The Grading System for Varicocele Size
Once diagnosed, your doctor will grade the varicocele with one of four grades:
| Grade | Description |
| Grade 0 | Subclinical: not palpable, detected only on ultrasound |
| Grade 1 | Small: palpable only during Valsalva manoeuvre |
| Grade 2 | Moderate: palpable without Valsalva, but not visible |
| Grade 3 | Large: visible through the scrotal skin and palpable |
How to Manage and Treat Varicocele
Many men do not need treatment for their varicocele. Most men can take over-the-counter pain relief medication such as ibuprofen or paracetamol (always check with your GP if you are taking any prescription medication). You may also find that supportive underwear that fits snugly may help with pain relief.
For those who have troublesome symptoms and in particular those with potential fertility issues, management options are as follows:
- Embolisation – where special thin metal coils are used to block the abnormal veins
- Surgery – where a cut in the groin or scrotum is used to close of the abnormal veins.
Undoubtedly symptoms are best managed by an individual patient-centred approach and some men would prefer surgery and others embolisation. When you are seen in rooms by the IR specialist you can trust that you will be only offered treatment if it is thought to be your best option.
Varicocele Embolisation
Varicocele embolisation is a non-invasive treatment option used to treat enlarged veins in a scrotum. It involves a thin tube introduced via a vein in the neck or groin and navigated to the veins inside the abdomen under x-ray guidance. Once in position special metal coils and sometimes foam is used to close the abnormal veins.
Embolisation is an excellent option as it means a varicocele can be treated without surgery. It does not involve any incisions or cuts on the groin or scrotum and does not need a general or spinal anesthetic. Surgery risks damage to the tube which carries sperm from the testicle. Risks from embolisation are very rare but can include blockage of other normal blood vessels.
Safe, effective treatments with less pain and quicker recovery.
Ensure you know all your options prior to invasive surgical treatment, schedule a consult with Dr Shaun Quigley.