Adenomyosis
What is Adenomyosis?
Adenomyosis is a condition where the lining of the womb extends abnormally deep into the uterus. The uterine tissue and cells grow deep in the muscular wall of the uterus and thickens it.
The displaced tissue will break down and bleed during a menstruation cycle, and this can cause discomfort and painful periods. It may also lead to abnormally heavy periods and bloating.
Adenomyosis is quite common - one study found anywhere from 20%-88% of women will experience symptoms.
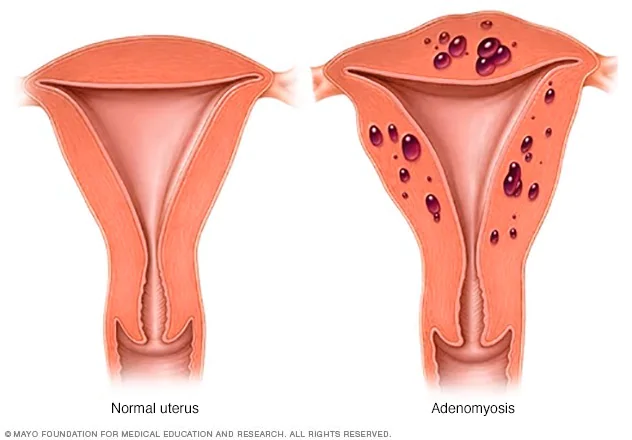
Image credit: Mayo Clinic
Adenomyosis Symptoms
Sometimes, adenomyosis produces no signs or symptoms, or only mild discomfort. However, when it does present symptoms, adenomyosis can result in:
- Heavy or prolonged periods
- Severe cramping or sharp, knifelike pelvic pain during menstruation
- Chronic pelvic pain
- Painful intercourse
- Tenderness or swelling in your abdomen (which may indicate an enlarged uterus)
One study found that the spectrum of severity of the clinical symptoms can vary from no symptoms (33% of respondents) to chronic pelvic pain (77%) and heavy menstrual bleeding (40 – 60%).

What Causes Adenomyosis?
We don’t know for sure. We know there is some link to endometriosis, a condition where cells from the lining of the womb are found outside the uterus. Adenomyosis often co-exists with fibroids, adenomyosis is routinely misdiagnosed as fibroids.
Despite this, some experts have developed a number of theories for what might cause adenomyosis:
- Tissue growth - some experts believe that endometrial cells, from the lining of the uterus, invade the muscle of the uterine walls.
- During development - some experts believe endometrial tissues ends up in the uterine muscle when the fetus is first formed.
- Childbirth - other experts believe a link exists between adenomyosis and childbirth, where inflammation of the uterine lining during postpartum periods can break the normal boundary of the cells that line the uterus.
- Stem cells - a recent theory proposes that bone marrow stem cells might invade the uterine muscle, causing adenomyosis.
What are the Risk Factors for Developing Adenomyosis?
Most cases of adenomyosis are found in women in their 40s and 50s. This could be due to longer exposure to estrogen than younger women, however recent research does suggest adenomyosis is just as common in younger women.
Risk factors for adenomyosis include:
- Prior uterine surgery, such as a C-section or fibroid removal.
- Childbirth
- Middle age

How is Adenomyosis Diagnosed?
Adenomyosis can be identified on transvaginal ultrasound but is often missed. An MRI of the pelvis is far more sensitive for detection of adenomyosis as well as allowing identification of all fibroids and other potential causes of symptoms such as endometriosis. This is usually the preferred method of diagnosing adenomyosis.
In most cases, since there is blood test for adenomyosis and a small biopsy (where a sample of tissue is taken to be examined) may miss an area of the condition, it is often only diagnosed after a hysterectomy and the uterus can be examined by a pathologist. This means adenomyosis is often misdiagnosed or simply missed.
Adenomyosis is often misdiagnosed as fibroids, since the symptoms are very similar.
Accurate diagnosis is important as this affects treatment options.
Adenomyosis and Fertility
When it comes to reproductive health, and conditions that affect these areas, one of the most common questions asked after receiving a diagnosis is, “can I still get pregnant?”
This is the topic of a lot of research and study, and there is a lot more to be done.
Despite this, studies have shown that the presence of adenomyosis can impact the endometrium’s receptivity and uterotubal transport.
In layman’s terms, adenomyosis can cause issues with the endometrium’s ability to function properly (this is required for the embryo to successfully implant on the uterine wall) and may make it difficult for semen to travel due to structural changes to the uterine wall caused by the condition.
Recent studies, using improved diagnostic tools, suggest that adenomyosis does have an impact on fertility, both spontaneous and assisted.
A recent meta-analysis found that during IVF, success rates were significantly lower in women in adenomyosis, and the risk of miscarriage was higher.
Unfortunately, there is still more to be understood about how adenomyosis contributes to infertility, and research in the area is ongoing.
Recommended Reading: The Impact of Adenomyosis on Fertility
Adenomyosis versus Endometriosis
While adenomyosis and endometriosis are similar, they are in fact two separate conditions. The major differences can be described as ‘inside vs outside’.
Adenomyosis: the cells that line your uterus grow deep inside the uterine wall and thicken it.
Endometriosis: the cells that line the uterus also grow on the outside. This can lead to issues with nearby organs such as your ovaries and the growth can breach them.
Discover more about the differences between adenomyosis and endometriosis.
Adenomyosis and Cancer
There are a number of studies and research papers linking adenomyosis and cancer.
A 2018 study found that women with adenomyosis are at a higher risk of developing endometrial and thyroid cancers. A 2020 study in the Journal of Cancer also found a link between adenomyosis and higher rates of endometrial cancer.
A 2021 study published in Gynecologic Oncology found a link between both endometriosis and adenomyosis with ovarian cancer, although it did state that the risk appears to be higher amongst women with endometriosis.
Adenomyosis and Weight Gain
Despite what you may hear, adenomyosis doesn’t directly cause weight gain. But a decrease in energy caused by adenomyosis may cause you to exercise less, and therefore gain weight (or have difficulty achieving weight loss) as a result. The weight difference between a healthy uterus and one with adenomyosis is negligible.
Adenomyosis and Estrogen Levels
As estrogen levels rise and fall during the menstrual cycle, the symptoms of adenomyosis also rise and fall, which is often why women who have adenomyosis, endometriosis or fibroids experience an increase in the severity of their symptoms while on their period.
Once a woman goes through menopause, and estrogen levels decline, you can usually expect symptoms to also decline. Therefore, it is common for women entering menopause to not require treatment for their adenomyosis.
It is also common for adenomyosis to be treated with birth control medication that restricts the production of estrogen and can pause the menstrual cycle.
Safe, effective treatments with less pain and quicker recovery.
Ensure you know all your options prior to invasive surgical treatment, schedule a consult with Dr Shaun Quigley.

Treating Adenomyosis
Only patients who are symptomatic need treatment. The majority of women with adenomyosis will not be symptomatic. It is also common for adenomyosis to go away after menopause, so treatment may depend on your stage of life.
When symptoms do occur they can be debilitating. If you are concerned by any of the following then you may wish to consider treatment:
- Heavy bleeding with frequent changes of pads
- Having to wear double pads
- Passing large clots
- Tiredness due to anaemia
- Concerns over periods limit your work, social life or normal activities
There are a range of treatment options, and finding the one best suited to you involves speaking with your doctor, or a specialist such as an Interventional Radiologist, to discuss your exact situation and needs.
How is Adenomyosis Managed and Treated?
For Mild Symptoms and Pain Management
Pain Management
If your symptoms are only mild, you may find that taking over-the-counter anti-inflammatories, such as ibuprofen, are the best option for you. Not only do anti-inflammatory medications relieve pain, but when taken just before your menstrual cycle begins they can help reduce blood flow.
Hormonal Treatment
Medications exist that can control estrogen production, and these can sometimes help relieve your symptoms:
- GnRH analogs like leuprolide (Lupron). These work by reducing the overall levels of estrogen, the hormone responsible for uterine tissue growth.
- Oral contraceptives like birth control pills. These can reduce blood flow and manage pain, although the research seems to suggest a IUD may be more effective.
- Progestin-only contraceptives like a pill, an injection, or an intrauterine device (IUD). These produce a hormone called progesterone which reduces bleeding, pain and shrinks the uterus and the adenomyosis by thinning the endometrial cells.
If You Are Not Planning a Pregnancy
If you have already given birth and are not planning to have any more children, there are surgical options available that can directly treat your condition.
Endometrial Ablation
Endometrial ablation is a procedure designed to destroy the uterine lining, the endometrium. It can be performed in a number of ways:
Freezing (cryoablation): Extreme cold is applied to the uterine tissue, and is done with the use of an ultrasound monitor to guide the healthcare specialist.
Heated balloon: at the other end of the temperature spectrum, heat can be used to destroy the uterine lining. A balloon filled with hot fluid is inserted into your uterus for 2 to 12 minutes, typically.
Heated free-flowing fluid: Heated saline liquid is allowed to flow freely throughout your uterus for around 10 minutes, destroying the uterine tissue.
Radiofrequency: Radiofrequency energy can also be used to destroy uterine tissue - a flexible device is inserted and the energy is emitted. This procedure is very quick, lasting only 1-2 minutes.
Microwave: Similar to radiofrequency, but requires a bit more time, usually 3-5 minutes.
Electrosurgery: For this procedure, you will be given general anesthesia. A telescopic device called a resectoscope and a heated instrument is used to see and remove uterine tissue.
In some cases, your healthcare provider may also recommend sterilization to prevent you falling pregnant in the future. Pregnancy after endometrial ablation can be complicated - an embryo can’t successfully implant without the uterine wall being thickened, and since your uterine tissue has been destroyed, but not removed, it is suggested you practice safe sex and continue to take birth control if you have not undergone sterilization.
After the procedure, your periods should lighten or stop completely within a few months.
Hysterectomy
When it comes to conditions involving female reproductive organs, it is often the case that the only ‘true’ solution is to remove the uterus completely.
While other treatment options exist, there is always a chance of the condition returning later. If you remove the uterus you remove this possibility.
However, a hysterectomy is not an option for someone still planning future pregnancies.
If You Are Planning a Future Pregnancy
For some women, treatment that destroys any reproductive organs or tissues is not acceptable, since planning a family is still a priority for them (or they at least want the option in the future). In this case, Uterine Artery Embolisation is our preferred treatment option.

Uterine Artery Embolisation
This minimally invasive approach is almost identical to Uterine Fibroid Embolisation, performed for uterine fibroids. This allows significant symptom control in a majority of patients and can prevent the need for hysterectomy. This procedure is performed by an Interventional Radiologist, is minimally invasive and avoids scar tissue developing in the uterus.
Safe, effective treatments with less pain and quicker recovery.
Ensure you know all your options prior to invasive surgical treatment, schedule a consult with Dr Shaun Quigley.